What are some commonly used psychiatric medications?
Depression is a very common disorder, affecting between five to ten percent of people, so we use antidepressants quite often. The medications we’ve been using for the past 25 years are called Selective Serotonin Reuptake Inhibitors (SSRIs). These newer generation drugs have much fewer side effects than those used in the past.
They do have some side effects though, the most common being gastric distress, nausea, headaches and insomnia. Some people also report sexual dysfunction and decreased libido. However, these side effects can be managed once the medication and dose is adjusted. SSRIs are usually more tolerated than older antidepressants.
Another group of drugs is the antipsychotics, which are used to treat schizophrenia and bipolar disorders. The second generation antipsychotics have fewer side effects than older ones, along with fewer cognitive effects and extrapyramidal side effects such as causing tremors or stiffness. However, side effects such as weight gain, increased blood sugar and increased cholesterol can occur with some of these drugs; these side effects need to be screened for on a regular basis

Is psychiatric medication an alternative to therapy? Or do they work hand in hand?
Medication and therapy usually work hand in hand. Being medication-compliant is another important part of the mental health recovery treatment as it helps bring stabilisation to the chemical and biological changes in the sufferer that cause the disorder.
For depression, we prescribe medication for moderate or severe symptoms if it’s causing impairment or distress. We also recommend psychotherapy in its various forms: cognitive behavioural therapy, dialectical behaviour therapy, acceptance and commitment therapy, interpersonal therapy or family therapy, depending on the psychosocial stressors.
For bipolar disorder or psychotic conditions like schizophrenia, medications are the mainstays of treatment. However, psychotherapy methods can also help with regulating emotions and give handles to help regulate distorted thoughts when mild symptoms occur. Psychological therapy also plays a role for Obsessive-Compulsive Disorder (OCD) and eating disorders. Here, psychotherapy has a much more important role.
What are some of the misconceptions people have about psychiatric medication?
The most common misconception is that all psychiatric medications make you feel like a zombie – you can’t function, you can’t go to work, your mental faculties are affected. While some of the older generation antipsychotic medications can cause mental fogginess, there are newer ones with fewer side effects. Some people also believe that if they start taking medication, they might become addicted. It is usually the benzodiazepine class of drugs that are addictive in the long term; antidepressants aren’t addictive in the long term. We also see many patients who’ve been taking medication on a long-term basis, but we work with them to minimise side effects. We do this by adjusting the dosage, changing the class of drugs used and lifestyle modification. It’s also worth mentioning that psychologists cannot prescribe any of these drugs, only psychiatrists can.
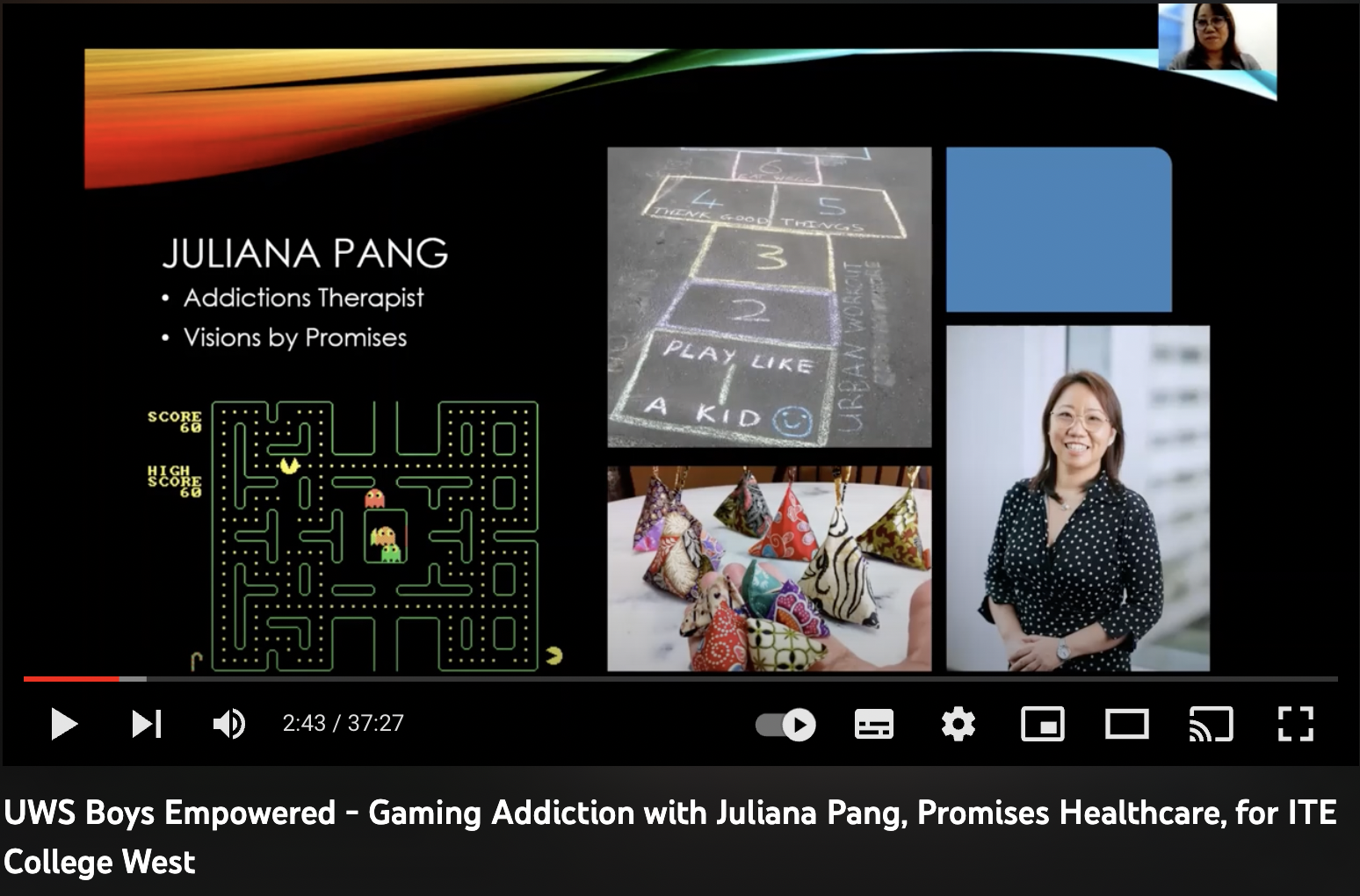
Can you tell us more about new techniques like Transcranial Magnetic Stimulation?
Transcranial Magnetic Stimulation (TMS) uses electromagnetic waves to stimulate the brain. Unlike electroconvulsive therapy, which is more for people with severe psychotic depression, TMS doesn’t require any sedation. The patient simply sits in a chair and has a device placed at specific parts of the brain where it sends small electromagnetic waves. It is an outpatient procedure and there aren’t usually any side effects.
TMS is used primarily for people with depression who haven’t responded to antidepressants or have severe side effects from medication. It’s not usually a first-line procedure.
Is it as effective as antidepressants?
It works in combination with them. If that alone isn’t helping, TMS can augment the medication. It can also help by itself, but once the treatment stops the patient can relapse, so it’s better to take medication along with it.
What are some psychiatric issues that people may not realise they have?
Many people don’t realise that depression or anxiety disorders are mental illnesses. They think it’s a weakness in their own personality or the result of external stressors they can’t handle. The stigma of mental disorders also plays a big part. People tend to be quick to seek help for physical issues but still feel uncomfortable seeing a psychiatrist. I think it’s becoming more accepted though. There’s a misconception that psychiatrists just provide medication.
What else do they do?
Psychiatrists work in teams. The team-based approach is very important because we have psychiatrists who are qualified doctors along with psychologists who are trained in psychotherapy. We also have social workers, case managers and occupational therapists.
It’s a misconception that psychiatrists cannot do therapy. There are many psychiatrists who are trained in many forms of therapy, but the psychologists are the professionals who study these critical areas in depth. We refer the patients to them because it is their area of expertise.
What would you tell someone who is unsure about seeking help?
Don’t be ashamed of your symptoms or be self-critical. Many feel their symptoms stem from a weak personality or an inability to handle stress. People need to understand that mental health issues can occur for people who’ve done everything right – people with a good job, a good family life, good support and no financial issues. Depression is a biological response and it can happen without any external stressors so there is no shame in seeking help.
Dr Rajesh is a Senior Consultant Psychiatrist at Promises Healthcare, a provider that offers a wide range of psychiatric and psychological services for patients of all ages. Promises is also the only private centre in Singapore to offer Transcranial Magnetic Stimulation.
For more information on psychiatric medication and treatments offered by Promises Healthcare, click here.
#09-22/23 Novena Medical Center | 6397 7309
This article first appeared in the February 2022 edition of Expat Living and was published on their website.